Mental Health Resources
Filter resources
Media Types
Topics
User Types

Anxiety around change and uncertainty
The webinar explores how young people navigate uncertainty, particularly during key life transitions and explores what anxiety is, its physical and mental effects, and its impact on daily functioning.

Asking for help (for adults)
Asking for help is a brave step. This guide offers actionable advice on how to ask for help and organisations that can offer support.
Asking for help (for young people)
Asking for help is a brave step. This guide offers actionable advice on how to ask for help and organisations that can offer support.

Autism and mental health
Whether you’re autistic, have a loved one who is autistic or work with autistic people, this webinar is a great insight into better understanding and enhancing the wellbeing of those with autism.

Building resilience in young people
Information and resources on the key themes around building resilience; sleep, movement, friendship, and self-compassion.

Coping with self harm
A guide for parents and carers on how to cope when your child is self-harming. Find out how to spot the signs and what you can do to help.

Coping with self harm (Welsh)
This guide offers information on the nature and causes of self-harm and how to support a young person for parents and carers in Welsh.

CoRAY mental health lesson plans
Our mental health lesson plans and resources are designed to help teachers and anyone who works with children and young people, and also by parents and carers have conversations about mental health topics.
CoRAY resources for parents and carers
Our mental health lesson plans and resources can be used by parents and carers to have conversations about mental health topics.

Early intervention in mental health
This webinar explores how to help children and young people build foundations for lifelong wellbeing. It highlights practical, evidence-based ways of supporting them to make sense of their experiences, feel capable of managing life’s challenges, and connect positively with others.

Five ways to wellbeing bookmark
Our colourful five ways to wellbeing bookmark is based on the 'Five Ways to Wellbeing' principle (NHS). It includes practical techniques to help you distract from worries and calm you mind.
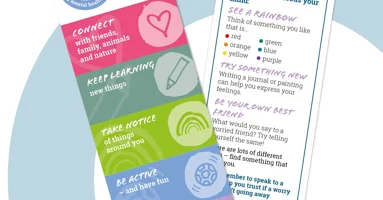
Five ways to wellbeing bookmark for children
Our colourful five ways to wellbeing bookmark for children is based on the 'Five Ways to Wellbeing' principle (NHS). It includes helpful techniques for when children are feeling worried.
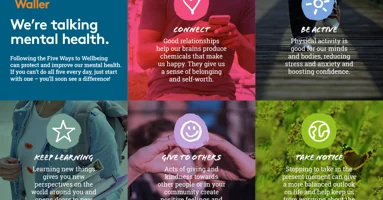
Five ways to wellbeing posters
Seven page poster pack - one for each of the Five Ways to Wellbeing plus two all-in-one designs.

In our own words
This is a package of resources for parents, carers, teachers, and others who want to support the mental health of children and young people.
Life at university poster
This A4 poster features a handy QR code directing students to a Charlie Waller page with guidance to support them through many common obstacles.

Life at university postcards
Support student mental health with these A6 postcards featuring a QR code linking to valuable guidance.

Making the move to university: care leavers
This guide is for care leavers going to university, it looks at how you can best access support and offers guidance on how to look after your mental health.

Making the move to university: international students
This resource covers everything you need to know about looking after your mental health if you're moving to another country for university.

Making the move to university: LGBTQIA+ students
This resource covers everything you need to know about looking after your mental health if you're moving to another country for university.

Making the move to university: not fitting in
This resource helps students or groups of students who feel as if they don’t fit in, by offering guidance on how to stay mentally healthy.

Making the move to university: Students with adverse childhood experiences
This guide is for young people who have had adverse childhood experiences, and offers support on how to look after your mental health when going to uni.

Making the move to university: young carers
This guide is for young carers and offers support on how to look after your mental health when going to uni as well as how you can best access support.

Managing stress and anxiety
This resource offers guidance on how to manage your time and stress levels ahead of exams or assessments, and strategies to help you keep yourself mentally well.
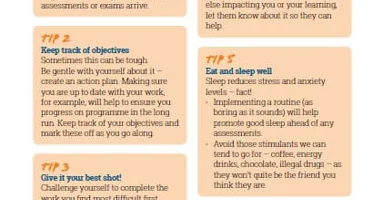
Managing stress and anxiety poster
This A4 poster offers the following six practical tips and pieces of advice on how students and apprentices can manage stress and prevent burn out.

Managing your mental health during exams
This guide offers some simple tips and reminders of how to take care of yourself when exam season approaches, and how to reach out for help and support if things get too much.

Navigating the first term of secondary school
In this webinar attendees will gain an understanding of the key anxieties young people face when moving to secondary school, develop positive strategies for support and sign-posting to useful resources such as the Charlie Waller Institute Resilience Rucksack.

Neurodiversity and mental health
In this webinar attendees will gain a better understanding of neurodiversity, learn about environmental adaptations that can positively impact people who are neurodivergent and understand what we can do to support the mental health of neurodivergent young people.

Perfectionism
This guide explains what perfectionism is, how it can be both healthy and unhealthy, and the impact it can have on wellbeing. It looks at ‘unhealthy perfectionism’ – how to spot it and advice on how to develop effective interventions.
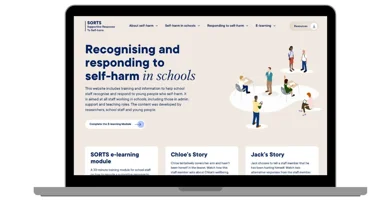
Recognising and responding to self-harm in schools
These resources include training and information to help school staff recognise and respond to young people who self-harm. It is aimed at all staff working in schools, including those in admin, support and teaching roles.

Results and clearing
The wait until results day often brings mixed emotions. Many students go through the clearing process. This guide will help you understand what to expect, how to adjust to changes, and maintain good mental health.

Schools' mental health policy template
A practical toolkit designed to help staff to develop a mental health policy for schools.

Self esteem and self confidence
In this webinar, you’ll learn about the factors that affect young people’s self-esteem, the difference between confidence and arrogance, signs of low self-esteem, and practical ways to help young people build healthy self-confidence.

Self harm: stories from parents and carers
Our video and advice provides guidance for parents and carers of young people who are self-harming and steps that you can take to help them.

Self harm: stories from those who work with young people
Our video and advice provides guidance for people who work with young people on steps that you can take to help them if they are self-harming.

Self harm: stories from young people
Our video and advice provides information for young people who are self-harming on understanding self-harm and where to get support.

Starting university: a guide for students
University can be fun and exciting but it can also be exhausting and challenging mentally. Take a look at our range of guidance about starting university and looking after your mental health.

Stepping forward
‘Stepping forward‘ is a unique stop-motion animation film about the transition between primary school and secondary school.

Supporting a child with anxiety
This guide provides parents and carers with helpful tips and strategies on how to support a child with anxiety.

Supporting a child with depression
This guide provides parents and carers with tips to help better support their child with depression.

Supporting a child with an eating problem
This guide provides parents and carers with helpful tips and strategies on how to support a child with an eating disorder or problem.

Supporting school transitions
Tips for parents and carers whose children are starting secondary school. They were provided by parents and carers with lived experience of supporting young people struggling with their mental health.

Supporting students’ mental health videos
These animations offer practical tips on how personal tutors and other academics can make a positive difference to students’ mental wellbeing.

Supporting your child with exam stress
This guide is designed to support parents and carers in helping their children manage exam stress and maintain good mental wellbeing. It provides practical advice on how to create a balanced approach to studying, recognise signs of anxiety, and offer encouragement.

Supporting your students with exam stress
This guide is designed to help educators support their students' mental health and wellbeing during exam periods. It offers practical advice on creating a nurturing school environment, recognising signs of anxiety, and promoting resilience.

Supporting a young person with thoughts of suicide
This webinar is for parents, carers, educators and anyone working with young people to gain a better understanding of suicide and how to support a young person who might be experiencing suicide thoughts.

Talking about self harm
This webinar is aimed at anyone who supports young people to learn what self harm is, the risk factors and practical guidance on how to support a young person who is self harming.

Talking about suicide for college staff
This resource equips staff with the knowledge to respond effectively and support students at risk of suicide and self harm. The guide builds confidence in addressing mental health concerns and creating a safe campus environment.

Talking about suicide for university staff
This guide helps university staff have a better understanding of suicide and self-harm. It aims to better equip them to respond and support someone who they are concerned may be at risk of suicide.

Talking with young people about suicide
This webinar is for anyone wanting to feel more confident talking to young people about suicide and suicidal ideation. You will learn about key risk factors, how to start conversations, recognise warning signs, and develop protective factors.

University mental health policy template
An evidence-informed toolkit for HE providers, giving guidance on creating an effective mental health and wellbeing strategy, as part of a whole institution approach.

Wellbeing Action Plan for Adults
Our Wellbeing Action Plan for Adults is designed to help you reflect on your emotional needs, how to look after yourself and where to seek help if you ever need it.
Wellbeing Action Plan for Children
Our Wellbeing Action Plan for children helps children identify their own challenges and what helps them. Designed for teachers of Key Stage 2 and 3, and to be personalised to enable children to build their own wellbeing toolkit.

Wellbeing Action Plan for Young People
Our Wellbeing Action Plan for young people is ideal for students attending sixth form or college, whether or not they have experienced mental health issues.It's a practical tool that helps students think about how to look after their mental health, when they may need support and where to seek help.

Whole School and College Approach
This webinar is for teachers and senior leaders to learn how culture change supports improved mental health and wellbeing in schools and colleges, the role of senior leadership in developing a positive approach, key areas for a whole organisational approach, and how to use the WSCA online toolkit.

Young people's emotional wellbeing
In this webinar, we explore what emotional wellbeing looks like, how emotions affect behaviour and wellbeing, signs a young person may be struggling, and practical strategies to support them.

Young people who self-harm
Developed by researchers at the University of Oxford, this guide includes information on the nature and causes of self-harm and how to support a young person who is self harming for school staff.